Can Thoracic Outlet Syndrome Cause High Blood Pressure
Overview
What is thoracic outlet syndrome?
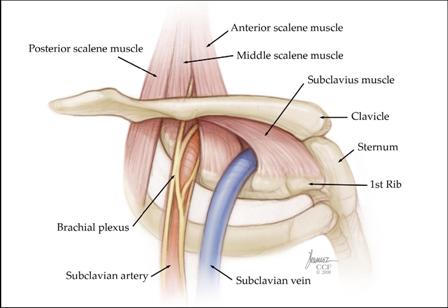
Thoracic outlet syndrome (TOS) is a term used to depict a grouping of disorders that occur when at that place is compression, injury, or irritation of the nerves and/or blood vessels (arteries and veins) in the lower neck and upper chest expanse. Thoracic outlet syndrome is named for the infinite (the thoracic outlet) between your lower neck and upper chest where this group of nerves and blood vessels is establish.
Who is afflicted by thoracic outlet syndrome?
Thoracic outlet syndrome affects people of all ages and gender. The condition is mutual amongst athletes who participate in sports that require repetitive motions of the arm and shoulder, such as baseball, swimming, volleyball, and other sports.
Neurogenic TOS is the near mutual form of the disorder (95 percent of people with TOS have this class of the disorder) and mostly affects middle-aged women.
Contempo studies have shown that, in general, TOS is more mutual in women than men, particularly among those with poor muscular development, poor posture or both.
Symptoms and Causes
What are the symptoms?
Download a Free Guide on Thoracic Outlet Syndrome
The signs and symptoms of TOS include neck, shoulder, and arm pain, numbness or dumb circulation to the affected areas.
The hurting of TOS is sometimes dislocated with the pain of angina (chest pain due to an inadequate supply of oxygen to the center muscle), but the two atmospheric condition tin can exist distinguished because the pain of thoracic outlet syndrome does not occur or increase when walking, while the hurting of angina usually does. Additionally, the pain of TOS typically increases when raising the affected arm, which does not occur with angina.
Signs and symptoms of TOS help determine the type of disorder a patient has. Thoracic outlet syndrome disorders differ, depending on the part(s) of the body they touch on. Thoracic outlet syndrome nigh normally affects the nerves, but the condition tin also impact the veins and arteries (least common type). In all types of TOS, the thoracic outlet infinite is narrowed, and there is scar formation around the structures.
Types of thoracic outlet syndrome disorders and related symptoms
- Neurogenic thoracic outlet syndrome: This condition is related to abnormalities of bony and soft tissue in the lower cervix region (which may include the cervical rib area) that compress and irritate the nerves of the brachial plexus, the complex of nerves that supply motor (movement) and sensory (feeling) role to the arm and paw. Symptoms include weakness or numbness of the paw; decreased size of hand muscles, which ordinarily occurs on one side of the body; and/or pain, tingling, prickling, numbness and weakness of the neck, chest, and artillery.
- Venous thoracic outlet syndrome: This status is caused by damage to the major veins in the lower cervix and upper breast. The condition develops of a sudden, often after unusual and tiring exercise of the arms. Symptoms include swelling of the hands, fingers and arms, as well every bit heaviness and weakness of the cervix and arms. The veins in the anterior (forepart) breast wall veins also may announced dilated (swollen).
- Arterial thoracic outlet syndrome: The least common, simply most serious, type of TOS is caused by congenital (present at nascence) bony abnormalities in the lower neck and upper chest. Symptoms include cold sensitivity in the hands and fingers; numbness, hurting or sores of the fingers; and poor blood circulation to the arms, hands and fingers.
What causes thoracic outlet syndrome?
The disorders caused by TOS are not well understood. Yet, information technology is known that when the claret vessels and/or nerves in the tight passageway of the thoracic outlet are abnormally compressed, they become irritated and can crusade TOS. Thoracic outlet syndrome tin exist a issue of an extra first rib (cervical rib) or an old fracture of the clavicle (collarbone) that reduces the space for the vessels and fretfulness. Bony and soft tissue abnormalities are among the many other causes of TOS. The following may increase the run a risk of developing thoracic outlet syndrome:
- Slumber disorders
- Tumors or large lymph nodes in the upper chest or underarm area
- Stress or depression
- Participating in sports that involve repetitive arm or shoulder movement, such as baseball, swimming, golfing, volleyball and others
- Repetitive injuries from carrying heavy shoulder loads
- Injury to the neck or back (whiplash injury)
- Poor posture
- Weightlifting
Diagnosis and Tests
How is thoracic outlet syndrome diagnosed?
Making a proper diagnosis is the most of import pace in TOS. Doctors who treat this condition include vascular surgeons, chest (thoracic) surgeons and vascular medicine physicians.
To diagnose your condition, your doctor will perform a consummate physical test and will review the results of previous diagnostic tests.
In some cases, a thorough evaluation past a skilled neurologist may be recommended to rule out cervical spine disease or other neurological conditions that may be mimicking or causing your symptoms.
Additional tests performed to diagnose thoracic outlet syndrome include:
- Nerve conduction studies (to evaluate the part of the motor and sensory nerves)
- Vascular studies (of the arteries or veins)
- Chest X-ray to rule out cervical rib abnormalities
- Cervical spine X-rays to dominion out a cervical rib (actress rib) or cervical (neck) spine abnormalities
- Computed tomography (CT) scan and magnetic resonance imaging (MRI) of the breast
- CT scan or MRI of the spine to rule out cervical spine impingement (force per unit area), which can mimic neurogenic thoracic outlet syndrome
- Magnetic resonance imaging with angiography (MRA) to view blood vessels
- Arteriogram/venogram (X-ray that uses dye to look at blood flow)
- Blood tests
Is thoracic outlet syndrome serious?
Although many cases of thoracic outlet syndrome (TOS) can't be prevented, the condition is treatable. If left untreated , TOS can crusade complications, such equally:
- Permanent arm swelling and pain (especially in patients with venous TOS)
- Ischemic ulcer of the fingers (open sore caused past reduced blood flow)
- Gangrene (the expiry of body tissue, frequently caused by a loss of blood flow)
- Blood jell
- Pulmonary embolism (obstruction in a blood vessel due to a blood clot)
- Neurogenic complications, such as permanent nerve harm
Management and Treatment
How is thoracic outlet syndrome treated?
Early on identification of TOS tin can help amend the success of treatment. Thoracic outlet syndrome treatments vary, depending on the blazon of TOS you lot have and your symptoms. The goals of treatment are to reduce symptoms and pain. Your health care provider will recommend the treatment option that is correct for you lot.
Before choosing any treatment, it is important to talk to your wellness care provider most the potential benefits, risks and side furnishings of your handling options.
Treatment of neurogenic thoracic outlet syndrome
- Physical therapy : The most common initial treatment for neurogenic thoracic outlet syndrome is physical therapy. Concrete therapy increases the range of motion of the neck and shoulders, strengthens muscles and promotes amend posture. Most patients experience an improvement in symptoms after undergoing concrete therapy.
- Medications: For hurting relief, over-the-counter pain medications, such as aspirin, acetaminophen (Tylenol), or ibuprofen (Motrin), may exist recommended. Your doctor may prescribe a muscle relaxant for additional pain relief.
- Surgery: In some cases, surgery may be needed to treat neurogenic thoracic outlet syndrome if symptoms proceed, despite an optimal class of physical therapy.
Treatment of venous thoracic outlet syndrome
To reduce the risk of blood clots and pulmonary embolism, treatment for venous thoracic outlet syndrome may include thrombolytic (clot-busting) or anticoagulant (blood thinning) medications and surgery. In many cases, the patient will be treated with thrombolytic medications and start anticoagulation therapy before surgery.
- Thrombolytic medications are given to deliquesce blood clots. This type of medication is e'er given to the patient in the hospital so he/she can be closely monitored. The medication(s) may exist injected straight into the vein or delivered via a catheter, a long slender tube, which is guided through the vein to the expanse where the blood clot is located. The jell-dissolving drug is sent through the catheter into the clot. The jell usually dissolves in a thing of hours to a few days. In some cases, the narrowed area of the vein will need to be treated with angioplasty (opening the vein using a balloon) to keep more clots from forming. Surgery is often recommended later on the clot in the vein has been finer treated/dissolved.
- Anticoagulant medications subtract the blood's ability to clot and keep more clots from forming. Anticoagulant medications include warfarin (Coumadin), heparin, low-molecular weight heparin and fondaparinux (Arixtra). You will receive information nigh how to take the anticoagulant medication that is prescribed for you lot.
- Surgery may be necessary along with medications to manage your symptoms. Surgery corrects the narrowing that is causing problems with the vein and may be recommended after the clot in the vein has been finer treated/dissolved with medications.
Treatment of arterial thoracic outlet syndrome
- Surgery: Patients with arterial thoracic outlet syndrome often crave surgical handling. Surgery may be performed to remove the first rib and make more than room for the vessels and nerves. Surgery may also be performed to repair whatsoever structural problems of the artery.
- Thrombolytic medications may be given before surgery, if necessary, to deliquesce blood clots. This type of medication is always given to the patient in the hospital so he/she tin can be closely monitored. The medication(s) may exist injected directly into the avenue or delivered via a catheter, a long slender tube, which is guided through the artery to the surface area where the blood clot is located. The jell-dissolving drug is sent through the catheter into the clot. The clot usually dissolves in a matter of hours to a few days. In some cases, the narrowed area of the artery volition need to be treated with angioplasty (opening the artery using a balloon) to prevent more clots from forming.
When is surgery necessary?
Although just x to 20 percentage of patients with TOS demand surgical handling, most patients with venous or arterial TOS will need surgical treatment.
Surgery for venous and arterial TOS is very effective. Among patients with venous TOS, elective surgery corrects symptoms in 90 to 95 percentage of cases; elective surgery resolves symptoms in more than 95 percentage of patients with arterial TOS.
Some patients with neurogenic TOS will need surgery. The primary goal of surgery in these patients is to remove the source of compression on the spinal fretfulness that supply stimulation to the arm, forearm and manus (the brachial plexus). This is typically achieved by removing the first rib, aberrant muscles or fibrous bands. If there is an extra rib causing compression, it may besides be removed.
Known as "decompression surgery," the procedure is typically completed by making an incision in the underarm surface area on the affected side. It can also exist performed through an incision made above the clavicle (collar bone). An alternative surgical approach known as video-assisted thoracoscopic surgery (VATS), which is performed through several minor incisions, may be used in some cases.
Surgical risks
Like all extensive surgical procedures, in that location are risks associated with decompression surgery. One significant take chances is failure to respond to surgery. In experienced centers, approximately fifty to 70 percentage of patients will accept improvement in their symptoms afterwards decompression surgery. For this reason, surgery to treat neurogenic TOS is reserved for those patients that remain debilitated despite appropriate noninvasive therapy, including supervised physical therapy and hurting relief. Other complications are rare, occurring in only two to 3 percent of cases, but include:
- Nervus injury
- Bleeding
- Pneumothorax (complanate lung)
- Lymphatic fluid leakage
Length of hospital stay
Following surgery, you volition stay in the hospital for ane night, and in some cases an additional day. During your recovery, you will begin physical therapy to you gain office and minimize pain and the recurrence of symptoms.
Resources
Doctors Who Treat
Doctors vary in quality due to differences in training and experience; hospitals differ in the number of services available. The more complex your medical trouble, the greater these differences in quality become and the more they matter.
Clearly, the doctor and hospital that you cull for complex, specialized medical care will accept a direct impact on how well you exercise. To assistance you make this option, please review our Miller Family Center, Vascular & Thoracic Institute Outcomes.
Cleveland Dispensary Heart, Vascular & Thoracic Institute Vascular Medicine Specialists and Surgeons
Choosing a doctor to treat your vascular affliction depends on where you are in your diagnosis and treatment. The post-obit Heart, Vascular & Thoracic Constitute Sections and Departments treat patients with all types of vascular disease, including claret clotting disorders:
Section of Vascular Medicine: for evaluation, medical management or interventional procedures to treat vascular affliction. In addition, the Non-Invasive Laboratory includes land-of-the art computerized imaging equipment to assistance in diagnosing vascular disease, without added discomfort to the patient. Telephone call Vascular Medicine Appointments, toll-free 800-223-2273, extension 44420 or request an engagement online.
Department of Vascular Surgery: surgery evaluation for surgical handling of vascular disease, including aorta, peripheral artery, and venous disease. Call Vascular Surgery Appointments, cost-gratis 800-223-2273, extension 44508 or request an appointment online.
Yous may also use our MyConsult second stance consultation using the Net.
The Middle, Vascular & Thoracic Institute besides has specialized centers and clinics to treat certain populations of patients:
- Aorta Center
- Thrombosis Center
- Lower Extremity Wound Clinic
- FMD Clinic
- SCAD Clinic
Larn more about experts who specialize in the diagnosis and treatment of vascular and arterial disease.
- See Almost U.s. to larn more almost the Sydell and Arnold Miller Family Middle, Vascular & Thoracic Institute.
Organizations
American Chronic Pain Association (ACPA)
P.O. Box 850
Rocklin, CA 95677-0850
Cost-free: 800.533.3231
Fax: 916.632.3208
Email: Website: theacpa.org/
National Rehabilitation Information Centre (NARIC)
4200 Forbes Boulevard, Suite 202
Lanham, MD 20706-4829
Phone: 301.459.5900
Toll-free: 800.346.2742
TTY: 301.459.5984
Fax: 301.562.2401
Email: Website: www.naric.com
Contact
If you demand more information, click here to contact us, conversation online with a nurse or call the Miller Family Center, Vascular & Thoracic Institute Resources & Information Nurse at 216.445.9288 or toll-complimentary at 866.289.6911. We would exist happy to assist you.
Becoming a Patient
- Make an engagement
- Programme Your Visit
- Billing & Insurance
- Visitor Civilities
Treatment Options
Boosted information near vascular handling options can exist constitute at:
- Vascular Surgery Services
- Aorta Surgery
- Carotid Avenue Disease Treatments
- Peripheral Avenue Disease Treatments
- Venous Disease Treatments
- IVC Filters for Claret Clot
- Visceral (Abdominal) Artery Disease Treatments
Handling Guides
- Aortic Aneurysm
- May Thurner Syndrome
- Thoracic Outlet Syndrome
- Vein and Vascular
- All Miller Family unit Heart, Vascular & Thoracic Constitute Treatment Guides
Diagnostic Tests
Diagnostic tests are used to diagnose your aberrant heartbeat and the almost constructive handling method.
- Diagnostic testing
Webchats
Our webchats and video chats give patients and visitors some other opportunity to enquire questions and interact with our physicians.
- Vascular Disease, Peripheral Arterial Disease & Thrombosis webchats and video chats
- All Miller Family Heart, Vascular & Thoracic Institute webchats
Videos
- Vascular Disease and Treatments Videos
- All Miller Family Heart, Vascular & Thoracic Constitute Videos
Interactive Tools
- Miller Family Centre, Vascular & Thoracic Plant Interactive Tools
Resource Links
- Recovery at home
- Support Groups and Data
- Visit Wellness Essentials* - Read articles on vascular disorders and healthy living on Wellness Essentials
- Follow Center, Vascular & Thoracic Institute webchats and news stories on Twitter*
- Subscribe to Middle, Vascular & Thoracic eNews
- American Stroke Association *
- American Middle Association *
- Vascular Cures*
- VascularWeb* - Resources for Vascular Affliction and Treatment
*A new browser window will open up with this link.
The inclusion of links to other websites does not imply whatever endorsement of the textile on those websites nor any clan with their operators.
Why choose Cleveland Clinic for your care?
Our outcomes speak for themselves. Please review our facts and figures and if you have any questions don't hesitate to inquire.
Source: https://my.clevelandclinic.org/health/diseases/17553-thoracic-outlet-syndrome-tos
0 Response to "Can Thoracic Outlet Syndrome Cause High Blood Pressure"
Post a Comment